10 ASC Patient Engagement Best Practices That Drive Results
- Brandon Daniell

- Feb 2
- 6 min read
Key ASC Patient Engagement Best Practices
Automated text reminders with a 98% open rate can reduce no-shows by 29% - use the 3-3-3 strategy (three weeks, three days, three hours) for best results
Digital intake forms paired with texted portal links cut day-of cancellations and boost completion rates by up to 89%
Intraoperative SMS updates to families achieve an 8.2/10 anxiety reduction score while decreasing staff interruptions
Structured post-discharge follow-up within 72 hours can reduce readmissions by up to 82% and post-op phone calls by 92%
Two-way texting cuts call volume by 50% and reduces average interaction time from 4-8 minutes to 30 seconds
OAS CAHPS surveys are mandatory for ASCs in 2025 - non-compliance triggers a 2.0 percentage point Medicare payment reduction
Before Surgery: Setting Patients Up for Success
Automated Reminders That Actually Get Opened
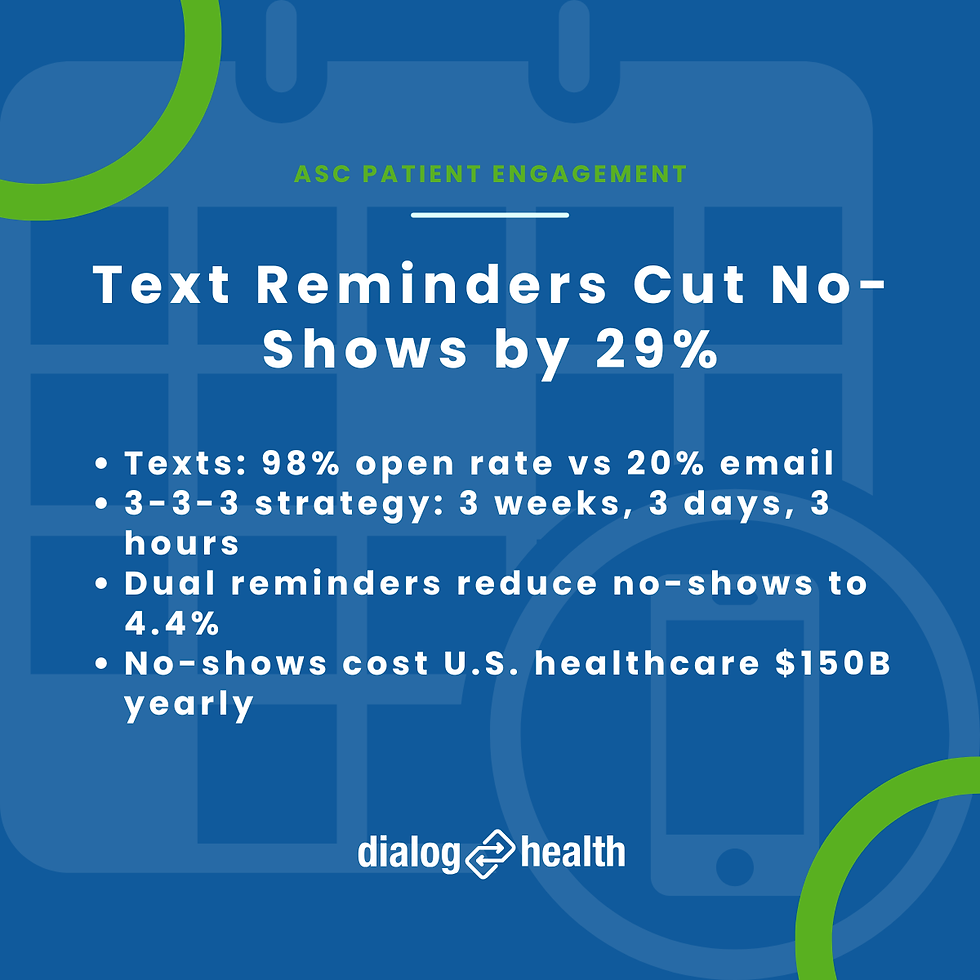
Patient no-shows cost U.S. healthcare $150 billion annually, with each missed surgical appointment representing roughly $200 in direct costs plus lost revenue.
The good news?
You can dramatically reduce this with the right reminder strategy.
Text messages achieve a 98% open rate compared to just 20% for email, which is why automated text reminders reduce no-shows by 29% according to MGMA surveys.
Timing matters just as much as the channel.
The 3-3-3 strategy has proven highly effective: send reminders at three weeks out (when confirmation rates are highest), three days before (giving patients time to reschedule if needed), and three hours prior to the procedure.
A study of 54,066 patients found that dual reminders at both 3 days and 1 day before reduced no-shows to 4.4%, compared to 5.3-5.8% for single reminders.
Here's another reason early engagement matters: same-day appointments see just a 2% no-show rate, while appointments booked 15 or more days out jump to 33%.
The longer patients wait, the more reminders they need.
Moving Paperwork Out of the Waiting Room
Digital intake forms save time on both sides.
Research shows 70% of patients complete them within 10 minutes, which translates to roughly 10 minutes of saved staff time per appointment.
The clinical impact is just as notable.
A study of 10,854 surgical cases at Macquarie University Hospital found that pre-admission clinics reduced last-minute cancellation rates and discharge delays.
Telehealth pre-anesthesia clinics using standardized protocols cut day-of-surgery cancellations from 3.38% to 1.72%.
One simple tactic that works: text patients a link to your portal.
One ASC saw an 89% increase in portal submissions just by texting links 5 days before appointments.
And with 40% of healthcare appointments booked after hours, mobile-optimized interfaces aren't optional anymore.
Preparing Patients for What to Expect
Between 75% and 80% of patients experience significant preoperative anxiety.
Multimedia education can help address this - 2024 research published in Scientific Reports found it significantly reduces preoperative anxiety in surgical candidates.
The benefits extend beyond comfort.
A systematic review found group preoperative education produced a 0.7-day reduction in mean length of stay and 44% lower odds of postoperative complications.
In bariatric patients specifically, video-based education reduced anxiety across 9 of 10 visual analog scale items, compared to just 5 of 10 for verbal and written instruction alone.
The challenge is that fewer than 40% of patients actually read paper instructions.
Digital reinforcement through text and video isn't a nice-to-have - it's the only way to ensure your education efforts stick.
Surgery Day: Keeping Families Connected

The hours a patient spends in surgery are often the most anxious for family members.
Automated SMS updates can bridge this gap without adding to staff workload.
A quality improvement initiative at Centre hospitalier de l'Université de Montréal studied this across 6,149 surgeries.
The program achieved a 75.6% participation rate and sent 34,129 messages - an average of 5.6 per surgery.
Messages went out at standardized checkpoints:
Check-in confirmation
OR entry
Procedure completion
PACU transfer
Discharge readiness
The results were strong: overall satisfaction reached 4.5 out of 5, and the anxiety reduction score hit 8.2 out of 10.
Among recipients, 96% said they felt more connected to their loved ones during surgery.
Staff benefited too - 87% found the system useful and efficient, noting fewer interruptions for verbal status updates.
After Discharge: The Critical Recovery Window
Why the First 72 Hours Matter Most
Nearly 19.6% of Medicare beneficiaries are readmitted within 30 days, costing the U.S. healthcare system $20 billion annually.
Many of these readmissions are preventable. In fact, 60% of hospital return visits after outpatient laparoscopic cholecystectomy stem from preventable events, with post-operative pain being the most common driver.
Timing your follow-up correctly makes a real difference.
Research suggests post-discharge day 2 may be optimal because it gives patients a full day of independent care, allowing for more accurate assessment of hydration, pain control, and self-care ability.
ERAS Society Guidelines recommend contact within 12-24 hours postoperatively.
The data backs this up: 70% appointment adherence was achieved among patients who received follow-up contact, versus just 34% for those with no contact.
In one of our case studies, a hospital surgical department reduced readmissions by 82% in just 90 days using two-way texting for Total Joint Replacement and Endoscopy patients.
The program also saved 20 staff hours and increased patient satisfaction from 83% to 100%.
Capturing Feedback That Drives Improvement
OAS CAHPS surveys became mandatory for ASCs in 2025.
If you're not compliant, you face a 2.0 percentage point reduction in Medicare payments.
CMS targets 200 completed surveys over 12 months per facility.
The effort is worth it beyond compliance. ASCs performing OAS CAHPS show 91.3% positive patient feedback on overall experience.
The survey measures several domains:
Preparation for surgery
Check-in processes
Facility cleanliness
Staff interactions
Discharge experience
Preparation for recovering at home
This feedback loop gives you actionable data to improve operations and patient satisfaction scores simultaneously.
Text Messaging Best Practices for ASCs
Staying HIPAA-Compliant

Standard SMS, iMessage, WhatsApp, and Facebook Messenger are not HIPAA-compliant.
You need a platform specifically designed for healthcare.
Compliant platforms must offer:
Business Associate Agreements
Encryption in transit and at rest
Access controls with audit trails
Role-based permissions
Never include protected health information in standard SMS - use secure links to patient portals instead.
Texting a patient's name alone isn't a HIPAA violation, but combining their name with health, treatment, or payment information is.
The "minimum necessary standard" applies: share only what's essential.
CMS updated its guidance in 2023 and now permits texting patient information when done through compliant secure platforms.
For consent, you need three elements:
Explicit written consent before sending any texts containing PHI
Risk disclosure warning about potential unauthorized disclosure
Easy opt-out mechanism (e.g., "Reply STOP to unsubscribe")
Timing and Content That Gets Results
95% of texts are read within 3 minutes, so timing your sends strategically matters.
The best times to send are 4 PM, 5 PM, 3 PM, and 9 AM - avoid lunch hours.
Keep messages to 160 characters or less for optimal readability.
Structure each message with: a greeting using the patient's first name, the purpose, key details, the action required, and contact information.
Include clickable links, date/time/location details, and phone numbers.
Avoid diagnoses or PHI, medical jargon, sending multiple messages at once, and vague next steps.
When your program delivers genuine value, opt-out rates typically stay under 10%.
Why Two-Way Texting Changes Everything
Two-way messaging delivers a 50% reduction in call volume.
That's because 91.9% of patients report that texts helped them avoid calling the office altogether.
The efficiency gains are significant.
An average text interaction takes 30 seconds versus 4-8 minutes for a phone call.
Two-way texting enables patient responses, interactive appointment confirmations, in-text question handling, and easy cancellation management.
The impact extends to revenue cycle too.
In one of our implementations, USPI used two-way texting for payment reminders and reduced outstanding accounts receivable from $110,000 to $48,000 - a 54% reduction in just six weeks.
Post-Op Texts That Prevent Readmissions
Penn Medicine documented a 55% decrease in 30-day readmission odds with automated texting, along with a 41% reduction in acute care resource use.
Patients who received and responded to texts were 32% less likely to be readmitted.
A structured post-op text workflow should include:
Day 0: Discharge confirmation
Day 1: Recovery check-in survey
Days 2-3: Medication reminders
Days 3-5: Activity and wound care reminders
Day 7: Symptom check
Days 7-14: Follow-up appointment reminder
After day 14: Satisfaction survey
Build escalation protocols into your workflow.
Flag pain scores above 7 for automatic nurse review, and route any "YES" responses to complication questions for priority callback within 2 hours.
A Dialog Health case study showed Baptist Plaza Surgicare reduced post-op phone calls by 92% through automated text surveys.
Over four months, this eliminated more than 3,250 calls and achieved a 2.5x reduction in staff workload - freeing nurses to focus on direct patient care.
Ready to Cut No-Shows and Readmissions at Your ASC?
The strategies above work - but only with the right platform behind them.
Dialog Health is a HIPAA-compliant two-way texting solution built specifically for healthcare.
We've helped ASCs achieve:
82% reduction in readmissions in just 90 days
92% reduction in post-op phone calls
54% increase in cash flow through automated payment reminders
Trusted by HCA Healthcare, AMSURG, and Ascension, our platform integrates with your existing systems and includes real-time analytics through AnalyticsPRO.
Here's what happens next: Fill out this quick form and one of our healthcare communication experts will reach out to schedule a 15-minute call.
No pressure - just answers.








