What are Patient-Reported Outcome Measures (PROMs): Full Guide
- Bo Spessard

- Jul 14, 2025
- 7 min read
Updated: Jul 16, 2025
Key Takeaways on Patient-Reported Outcomes (PROs)
PROs measure patients' health status directly from their perspective without third-party interpretation, capturing subjective aspects that clinical tests might miss.
Tools used for PROs (PROMs) include both generic instruments (like EQ-5D-5L) that assess overall health and condition-specific measures that target particular diseases and symptoms.
The use of PROs at individual, organizational, and system levels transforms healthcare delivery by putting patient experiences at the center of clinical decision-making.
PROs allow healthcare providers to identify problems earlier, personalize treatment plans, and evaluate service quality against other providers, ultimately improving quality of patient care.
When successfully implemented, patient-centered care supported by PROMs leads to better communication between patients and providers, with studies showing improved patient outcomes including higher survival rates and fewer emergency visits.
Fundamentals of Patient-Reported Outcome Measures
Defining Patient-Reported Outcome Measures

Let's talk about prom - no, not the high school dance - but patient-reported outcome measures (PROMs).
These are questionnaires that collect health status information straight from patients without anyone else interpreting what they say.
When a patient fills out a survey about their symptoms or quality of life, they're providing patient-reported outcomes that help doctors understand what matters to them.
Unlike lab tests or doctor observations, patient-reported outcomes capture the subjective side of health.
These measures help us understand what patients experience in their day-to-day lives.
They give us a window into patient outcomes that clinical tests might miss.
Think of them as a direct line to what patients are feeling about their health status and how their condition affects them.
Types of PROMs: General and Condition-Specific Tools
PROMs come in two main flavors: generic instruments that work for anyone, and condition-specific tools designed for specific conditions.
Generic tools look at your overall health regardless of what disease you might have.
They focus on things like health-related quality of life and functional abilities - can you climb stairs? Sleep through the night?
These tools (like EQ-5D-5L or SF-36) help compare people with different conditions.
On the flip side, condition-specific tools zero in on particular diseases.
They measure illness severity and health aspects that relate to certain patient experiences.
If you have anxiety, a tool like GAD-7 asks questions specifically about anxiety symptoms.
These tools dig deeper into how a specific condition affects your life.
Most doctors use both types together to get the full picture of a patient's health.
Relationship Between PROs and Patient-Reported Experience Measures (PREMs)
While PROs tell us about outcomes, there's another tool called patient-reported experience measures (PREMs) that focus on the healthcare experience itself.
Did the doctor listen to you? Was the waiting room comfortable?
These questions collect patient experience data about the quality of care rather than the results.
Research shows these two things connect in interesting ways.
Good patient outcomes can boost experience ratings by up to 10%.

And when patients receive more patient-centered care, their outcome scores typically improve by about 3%.
Healthcare providers who want the complete picture often look at both - what happened during care and what results patients got afterward.
Multi-Level Applications: From Individual Care to Healthcare Systems
PROs work at different levels throughout healthcare.
For individual patients, they help doctors identify problems and assess how well treatments work.
For organizations, care providers use them to check service quality and see how they stack up against other providers.
At the system level, they inform how healthcare resources get distributed within a broader framework.
Every healthcare organization from small clinics to major hospitals can use this information to evaluate their performance.
These tools allow healthcare teams to personalize care based on what matters to each patient.
They also help spot problems early - before they become serious - and give patients more say in their treatment decisions.
Some countries have made PROs part of national policy. In the UK, for example, the government requires them for four common surgical procedures.
This helps identify when surgery is truly needed and creates ways to reward hospitals for good outcomes.
Implementation and Utilization of PROs
Developing and Selecting Appropriate Measurement Tools

If you're thinking about using PROs, selecting the right tools matters.
You'll want validated surveys with solid measurement properties that fit your patients.
Good tools go through a careful development process with real patient input.
Think of it as product testing - they generate questions, test them out, validate the results, and fine-tune until they work well.
Most healthcare teams find it easier to use existing validated questionnaires instead of starting from scratch.
When picking a tool, look at who it was designed for, what it measures, its validity, and any limitations that might affect your results.
Don't forget practical concerns like reading level and language options. The optimal tool works for all your patients, regardless of their education or background.
Data Collection Methodologies and Technology Platforms
Once you've picked your tools, you need to figure out how to collect the data.
Should patients fill out forms in the waiting room? Get surveys in the mail? Answer questions via text message?
For the most honest feedback, patients should complete questionnaires away from their clinician.
Many hospitals now use text messaging for patient reported data collection because it's convenient and boosts response rates.

Technology has made collection easier through online forms and conversational interfaces.
Just make sure whatever system you use works for patients with different literacy levels and keeps their information secure.
Analyzing and Interpreting PROs Data
After you've collected responses, the real work begins - making sense of what patients told you.
Many hospitals track patients over time, linking pre-procedure and post-procedure questionnaires to see how things changed.
When comparing different doctor groups or hospitals, you need to adjust for patient differences to avoid bias in your interpretation.
Remember that a patient's experience provides context that numbers alone might miss.
Sometimes what patients report differs from clinical measurements.
This doesn't mean either one is wrong - they're just capturing different aspects of care.
Good analysis considers both perspectives.
Integration into Clinical Decision-Making
The hardest part of implementing PROs often isn't collecting data - it's getting doctors to actually use it.
When done well, this information helps make better treatment decisions and improves patient well-being through earlier problem detection.
For success, you need good training programs and strong administrative support.
Your electronic records should make PRO data easy to access when making decisions.
Many doctors underestimate how much this information can improve care.
Studies show that 75% of nurses report better patient care when using PROs, and 65% of oncologists make better treatment choices with this information at hand.
Impact, Benefits and Challenges
Enhanced Patient-Centered Care and Communication
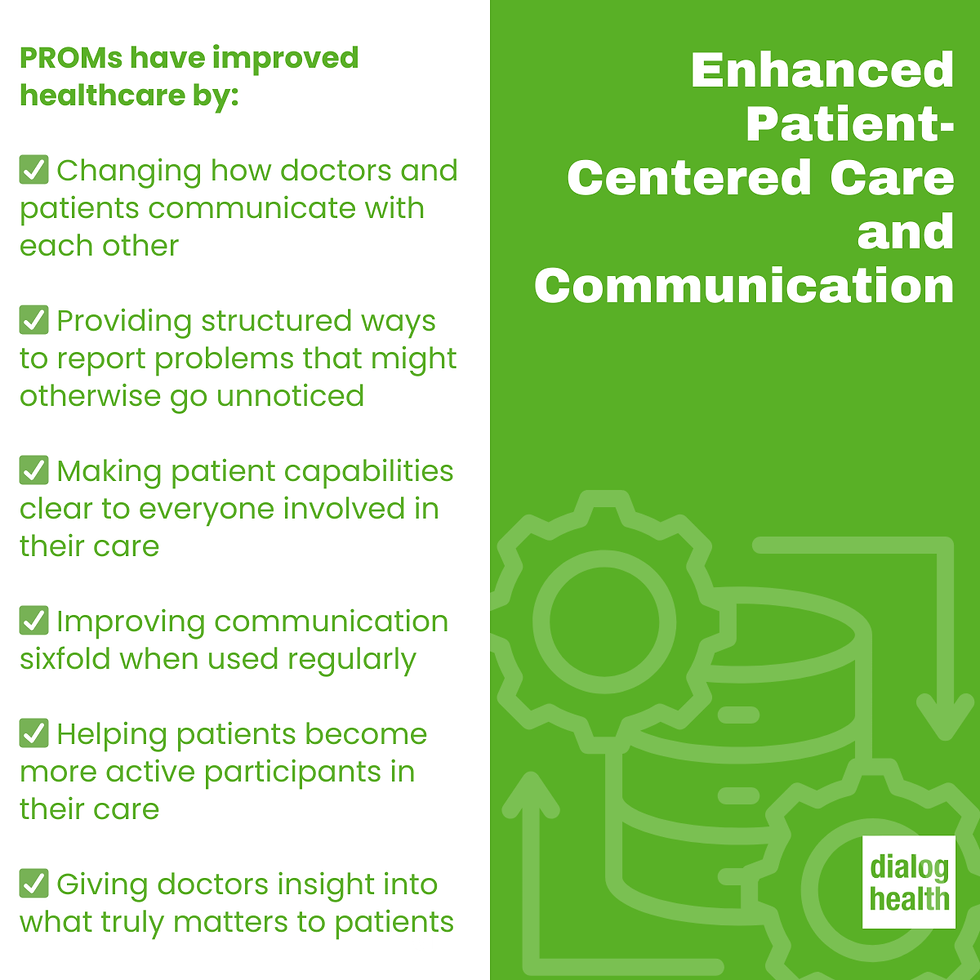
PROMs have changed how doctors and patients talk to each other.
They're used to collect information about symptoms, mobility, and recovery in all kinds of settings - from surgical units to outpatient clinics to discharge planning.
For patients going through chemotherapy or recovering from surgery, these tools provide a structured way to report problems that might otherwise go unnoticed.
They help make what's feasible for each patient clear to everyone involved in their care.
Studies show communication improves sixfold when teams regularly use PROs.
Patients become more active in their care, and doctors gain insight into what really matters to those they treat.
Improved Clinical Outcomes and Resource Utilization
The benefits go beyond better conversations.
Cancer patients whose care included PROs had a 10% higher survival rate in one major study.
These tools help catch symptoms earlier and reduce unnecessary hospital visits.
According to research, digital health monitoring with PROs cut emergency visits by 25% and hospital admissions by 38%.
That translates to real savings for both patients and hospitals.
Rather than creating extra work, well-implemented PROMs actually save resources by focusing care where it's needed most.
Hospitals find they can reward teams that consistently deliver good outcomes, creating positive incentives for improvement.
Implementation Barriers and Standardization Issues
Despite the benefits, challenges exist.
Research tools don't always work well in busy clinics.
Patients might give different answers depending on when and how you ask questions.
Language and literacy create hurdles too.
Translation costs limit multilingual options, potentially excluding patients who need them most.
Implementation costs money - for training, technology, and analysis.
Perhaps most troubling, even when hospitals collect good data, doctors don't always use it.
One study found only 1% of physicians regularly looked at available patient reports when making decisions.
Future Directions and Emerging Applications

Looking ahead, the picture brightens.
New AI techniques will soon make patient responses more meaningful.
Automated systems will deliver insights to the right people at the right time.
Better electronic record integration will put information at doctors' fingertips.
Text messaging systems will keep outpatients connected to their care teams with personalized communication.
Mobile health apps and wearable technology will expand what's feasible, especially for outpatient monitoring.
As techniques improve, we'll see better tools that work for diverse patient groups across cultural and language barriers.
Transform Your PROs Implementation with Dialog Health
Are you struggling with collecting patient-reported outcomes?
PROMs are essential for patient-centered care, but implementation challenges can be daunting:
Low response rates from traditional collection methods
Difficulty gathering data between visits
Integration issues with clinical workflows
Resource constraints for consistent follow-up
Dialog Health's two-way texting platform meets patients where they are - on their mobile phones.
Our healthcare-specific solution helps you:
Significantly increase response rates with convenient text-based surveys
Simplify collection with automated outreach at key points in the care journey
Improve clinical workflows with real-time symptom alerts
Reduce administrative burden through streamlined processes
Healthcare organizations using Dialog Health report earlier symptom detection, reduced emergency visits, and improved patient satisfaction.
 | Written by Bo Spessard Bo brings the perspective of both an entrepreneur-operator and trusted advisor to Dialog Health. He spent 5 years as a corporate attorney and 15 years leading fast-growing B2B SaaS companies. His expertise expands enteprise software, scaling sales organizations and empowering staff to deliver exceptional client services. He was COO of Emma, a B2B SaaS marketing company which was acquired by Insight Partners in 2018. Since Emma, he has advised multiple companies through transition, growth and fundraising. At Dialog Health, he is leading Sales & Marketing and doing his level best to bring corduroy back from the 1970s. |
|---|








